Introduction
Physiotherapy in Baie Verte and Springdale for Foot Issues
Welcome to Body Works Fitness & Physiotherapy’s resource on Adult Acquired Flatfoot Deformity.
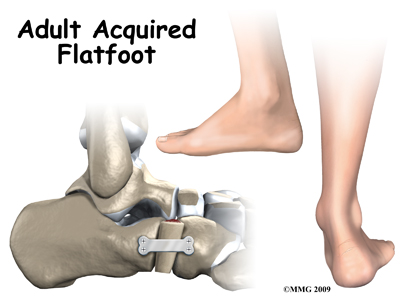
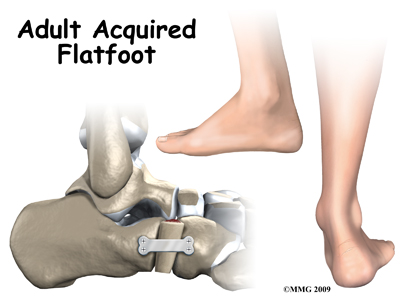
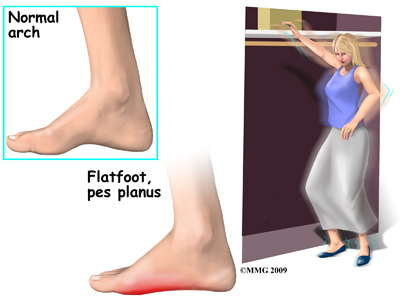
Adult acquired flatfoot deformity (AAFD) is a painful condition resulting from the collapse of the longitudinal (lengthwise) arch of the foot. As the name suggests, this condition is not present at birth or during childhood. It occurs after the skeleton is fully matured.
In the past this condition was referred to as posterior tibial tendon dysfunction (or insufficiency) but the name was changed because the condition really describes a wide range of flatfoot deformities, not just those caused by posterior tibial tendon dysfunction. AAFD is most often seen in women between the ages of 40 and 60.
This guide will help you understand:
- how the problem develops
- how health care professionals diagnose the condition
- what treatment options are available
- what Body Works Fitness & Physiotherapy’s approach to rehabilitation is
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Foot therapy|limit:15|heading:Hear from some of our *Foot Therapy* patients#
Anatomy
What parts of the foot are involved?
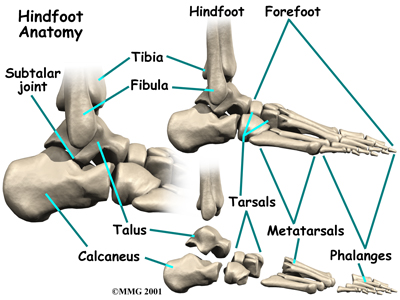
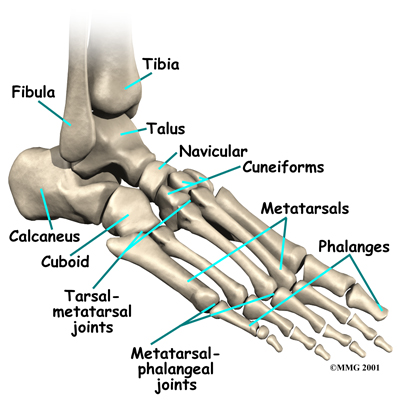
The skeleton of the foot centers around the talus, or ankle bone, which forms the main part of the ankle. The two bones of the lower leg, the large tibia and the smaller fibula, come together around the talus to form a very stable structure.
The two bones that make up the ‘hindfoot’ include the talus and the calcaneus, or heel bone. The talus is connected to the calcaneus at the subtalar joint. The ankle joint where the talus connects to the tibia and fibula allows the foot to bend up and down. The subtalar joint allows the foot to rock from side to side.
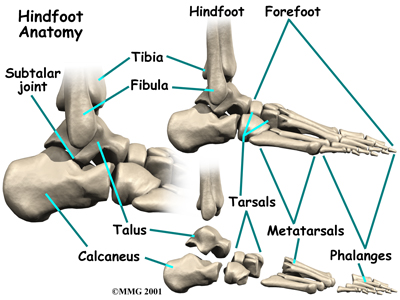
Just down the foot from the ankle is a set of five bones called tarsal bones that work together as a group. These bones are unique in the way they fit together. There are multiple joints between the tarsal bones. When the foot is twisted in one direction by the muscles of the foot and leg, these bones lock together and form a very rigid structure. When they are twisted in the opposite direction, they become unlocked and allow the foot to conform to whatever surface the foot is contacting.
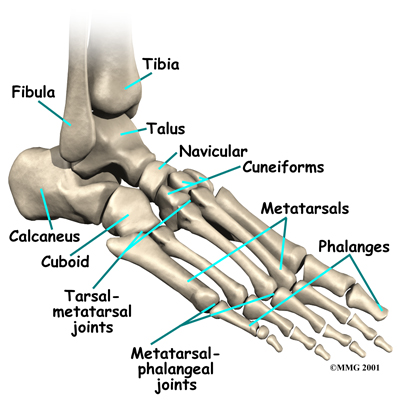
The plantar fascia is a thick band of tissue on the bottom of the foot that extends from the heel to the toes. When you pull your toes back with one hand, you will be able to feel this band with your fingers of the other hand. This fascia is also critical in supporting the long arch of the foot and in creating the rigid foot structure mentioned above.
The tarsal bones are connected to the five long bones of the foot called the metatarsals. The two groups of bones are fairly rigidly connected, without much movement at the joints.
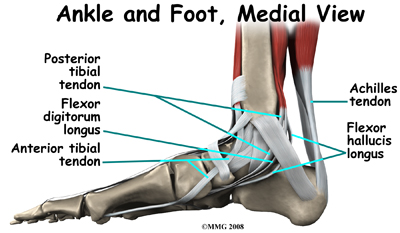
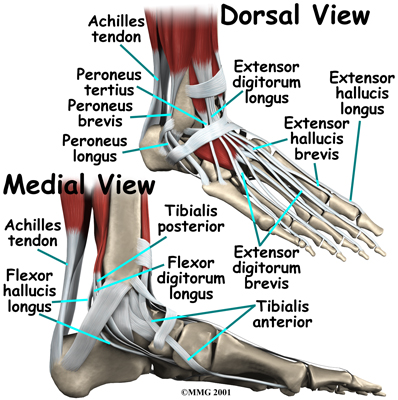
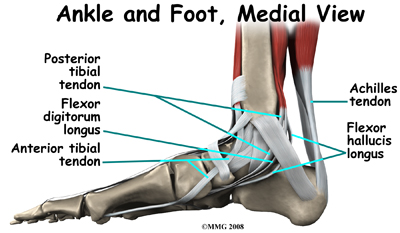
The large Achilles' tendon, at the back of the ankle, is one of the most important tendons for walking, running, and jumping. It attaches the calf muscles to the heel bone to allow us to rise up on our toes. The posterior tibial tendon attaches one of the smaller muscles of the calf to the underside of the foot. This tendon helps support the arch and allows us to turn the foot inward. Failure of the posterior tibial tendon is a major problem in many cases of AAFD.
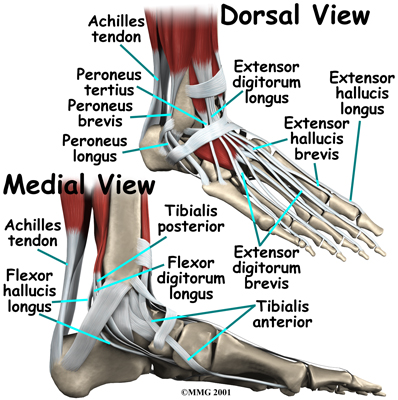
Foot Anatomy Ligaments & Tendons
The toes have tendons attached on the bottom of the foot that bend the toes down and also tendons that straighten the toes (on the top of the toes.) The anterior tibial tendon (tibialis anterior) allows us to pull the foot up, like you are taking your foot off the gas pedal. Two tendons, called the peroneal tendons, run behind the outer bump of the ankle (called the lateral malleolus.) These tendons help turn the foot outward.
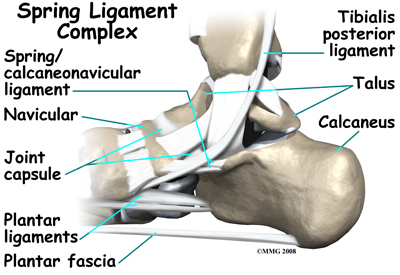
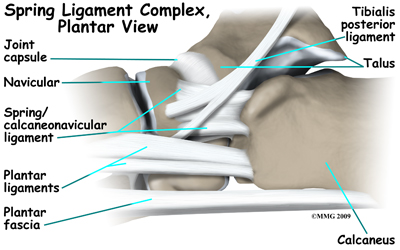
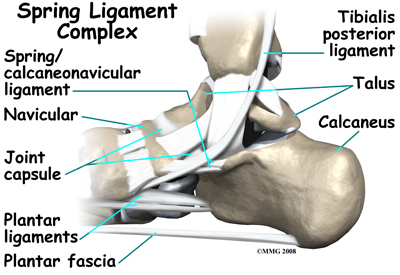
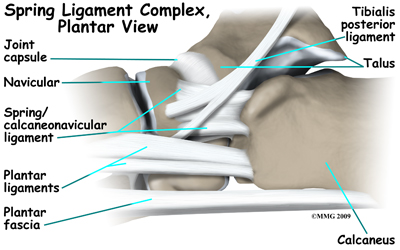
Many small ligaments hold the bones of the foot together. Most of these ligaments form part of the joint capsule around each of the joints of the foot. A joint capsule is a watertight sac that forms around all synovial-type joints. The capsule is made up of the ligaments around the joint and the soft tissues between the ligaments that fill in the gaps and form the sac.
The spring ligament complex is often involved in AAFD. This group of ligaments supports the talonavicular joint. The spring ligament complex works with the posterior tibial tendon and the plantar fascia to support and stabilize the longitudinal arch of the foot.
Related Document: Body Works Fitness & Physiotherapy's Guide to Foot Anatomy
Causes
What causes AAFD?
There are multiple factors contributing to the development of this problem. Injury to the nerves of the foot, laxity (looseness), or dysfunction of the spring ligament and tendon structures on the medial side of the foot, such as the posterior tibialis tendon, can all result in deformity of the foot and/or ankle resulting in AAFD. Subluxation (partial dislocation) of the subtalar or talonavicular joints can occur. A bone fracture is also a possible cause. The resulting joint deformity from any of these problems can lead to AAFD.
Dysfunction of the posterior tibial tendon has always been linked with AAFD. The loss of active and passive pull of the tendon alters the normal biomechanics of the foot and ankle.
The reasons for this can be many and varied as well. Diabetes, high blood pressure, and prolonged use of steroids are some of the more common causes of AAFD brought on by impairment of the posterior tibialis tendon. Overstretching or rupture of the tendon from a traumatic activity can also result in tendon and muscle imbalance in the foot leading to AAFD. Loss of blood supply for any reason in the area of the posterior tibialis tendon is another factor.
Rheumatoid arthritis is also one of the more common causes of AAFD. About half of all adults with this type of arthritis will develop AAFD over time. In such cases, the condition is gradual and progressive due to the laxity in the ligaments that accompanies this type of arthritis.
Obesity has also been linked with this condition. The excess weight causes pressure on the foot, which causes the arch to drop. Misalignment of the lower extremities in obese patients also contributes to the deformity. It should be noted that poor alignment of the lower extremities, in anyone, obese or not, can also progressively lead to AAFD.
Symptoms
What does this condition feel like?
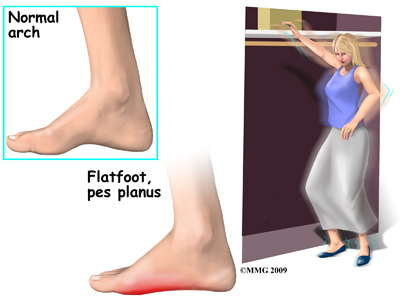 At first you may notice pain and swelling along the medial (big toe) side of the foot. This is where the posterior tibialis tendon travels from the back of the leg under the medial ankle bone to the foot. As the condition gets worse, tendon failure may occur, and ligament laxity will worsen, causing the pain to get worse. Some patients also experience pain along the lateral (outside) edge of the foot and ankle, particularly as a deformity develops.
At first you may notice pain and swelling along the medial (big toe) side of the foot. This is where the posterior tibialis tendon travels from the back of the leg under the medial ankle bone to the foot. As the condition gets worse, tendon failure may occur, and ligament laxity will worsen, causing the pain to get worse. Some patients also experience pain along the lateral (outside) edge of the foot and ankle, particularly as a deformity develops.
You may find that your feet hurt at the end of the day or after long periods of standing. Some people with this condition have trouble rising up on their toes. They may be unable to participate fully in sports or other recreational activities.
Shoes that have an arch support may relieve your pain, whereas going barefoot will likely increase your discomfort.
Diagnosis
How do health care professionals diagnose the problem?
The history and physical examination are probably the most important tools that health care professionals, including your physiotherapist at Body Works Fitness & Physiotherapy, will use to diagnose this problem. The wear pattern on your shoes can offer some helpful clues as it shows wear and tear on the medial sole rather than the lateral posterior sole, which would be normal. The alignment of your hips, knees, ankles and feet will be observed in both standing and sitting. You may be asked to twist your body with your feet planted on the ground, squat, or walk without shoes so your therapist can observe your feet and arches as you move.
Your therapist will also assess the position and mobility of the bones of your feet to determine if there is any subluxation, laxity, or even stiffness in any part of the ankle or foot which may be contributing to your problem.
The strength in the muscles of the foot and lower leg will also be assessed. In addition, your physiotherapist will assess the strength in the muscles of your hip, as these muscles also play a part in controlling the alignment of your lower leg as well as lifting the arch of your foot. The biomechanical link between the hip and foot can be felt if you stand relaxed and squeeze both buttocks muscles together. As you do this you will feel the arches of your feet slightly lift. It is for this reason that control around the foot cannot only be left to the joints and muscles directly connected to the foot. The strong hip muscles will also need assessing and addressing if they are shown to be weak or inadequately functioning.
Muscle testing helps identify any areas of weakness or muscle impairment and imbalance. This will be done in both the weight bearing and non-weight bearing positions. An important test that can help identify insufficient posterior tibial tendon problems is the single heel raise. You therapist will ask you to stand on one foot and rise up on your toes. You should be able to lift your heel off the ground easily while keeping the heel bone (calcaneus) centered and slightly turned inward (inverted) and your knees straight. If you cannot, your posterior tibialis muscle and tendon may be impaired.
X-rays are often used to study the position, shape, and alignment of the bones in the feet and ankles. Magnetic resonance (MR) imaging is the best modality for evaluating the posterior tibial tendon and spring ligament complex of the medial foot, and to determine the stage of injury progression.
There are four stages of AAFD. The severity of the deformity determines your stage.
Stage I: There is a flatfoot position but without any deformity. Pain and swelling from tendinitis is common in this stage.
Stage II: There is a change in the foot alignment. This means a deformity is starting to develop. The physician or therapist can still move the bones back into place manually (passively).
Stage III: There is a fixed deformity. This means the ankle is stiff or rigid and doesn’t move beyond a neutral (midline) position.
Stage IV: Is characterized by deformity in the foot and the ankle. The deformity may be flexible or fixed. The joints often show signs of degenerative joint disease (arthritis).
Body Works Fitness & Physiotherapy provides services for physiotherapy in Baie Verte and Springdale.
Treatment
What treatment options are available?
Nonsurgical Treatment
Conservative (non-operative) care is advised as the first line of treatment. A simple modification to your shoe may be all that’s needed in the early stages of this injury. Sometimes purchasing shoes with a good arch support is sufficient. For other patients, an off-the-shelf (prefabricated) shoe insert or orthotic works well.
Alternatively, a customized orthotic is designed specifically for your foot and positions it in proper alignment. Like the prefabricated insert, the orthotic fits inside your shoe. These often work well for mild to moderate deformity or symptoms.
Your physician may suggest over-the-counter pain relievers or anti-inflammatory drugs such as ibuprofen to assist with the pain. If symptoms are very severe, a removable boot or cast may be used to rest, support, and stabilize the foot and ankle while still allowing function. Patients with a longer duration of symptoms or a greater deformity may need a customized brace. The brace provides support and limits ankle motion. After several months, the brace is replaced with a foot orthotic.
Nonsurgical Rehabilitation
Physiotherapy at Body Works Fitness & Physiotherapy is an important part of treating and resolving AFFD particularly in the early stages of development, when the foot remains flexible.
On your initial treatment at Body Works Fitness & Physiotherapy your physiotherapist will first focus on relieving your pain. They may use ice, heat, ultrasound, or other electrical modalities on the bottom of your foot or along your shin to provide you with relief. Icing or heating your arch at home will provide similar relief. Your physiotherapist may massage the bottom of your foot or calf, which can be particularly useful in relieving your discomfort. Unfortunately these treatments only provide temporary relief; addressing the real problem of the fallen arch and misalignment, will provide more long-term relief to your injury.
Physiotherapy exercises will begin with strengthening exercises for your foot and posterior tibialis muscle. As mentioned above, these muscles work to lift the arch of the foot, along with the muscles of the hip, which control alignment down the lower leg chain, and also assist in lifting the arch of the foot. A Theraband may be used to provide added resistance to the muscles of the foot, and to strengthen the hip muscles. Your therapist may also prescribe stretching exercises, particularly for the muscles of your calf, which, when tight, can force the foot out of alignment. When performing all stretches it is imperative that you maintain good alignment of your foot and arch so as not to compound the forces going through your already flattened arch.
Being that AAFD develops over time, it is common for patients to not even notice how flat their feet are. The position of your feet becomes the ‘new normal.’ Re-learning the proper position of your arch is crucial to relieving the pain caused by AAFD as well as stopping the progression of any deformity. Proprioception is the term used to describe one’s sense of joint position. Your physiotherapist will teach you what the correct position of your foot and arch should be and will give you exercises that challenge the proprioception of your knee, foot, ankle, and arch. Initially these exercises may be while you are sitting but as you progress, your physiotherapist will advance your exercises so you are doing them in standing, and eventually just on one foot at a time. The standing position is an important position to work up to as it is much more functional in mimicking normal everyday activities such as walking or stair climbing. Eventually your physiotherapist will prescribe exercises that are extremely challenging, especially if you are involved in a high-level sport. Exercises such as squatting and jumping will be added and you will be required to do these activities while maintaining proper foot and leg alignment, as well as arch control.
If you have not already invested in some orthotics to assist with lifting your arch, your physiotherapist will advise you on whether you should purchase some, and where to do this. Often taping the bottom of the foot, which your physiotherapist can do, and can teach you to do on your own, can be trialed before expensive orthotics are purchased. Taping may be enough in mild cases of AAFD, as long as you can learn to control the position of your foot and maintain this position during high-level activities. In most cases shoe inserts, even pre-fabricated ones, will significantly improve the symptoms of AAFD, and will be recommended to both relieve symptoms and to avoid future progression of the injury. Custom fit orthotics are recommended for any individuals who have a significant foot drop, or for whom prefabricated ones do not relieve their symptoms.
As mentioned above, excess weight will add to the problem of AAFD, so if you are obese or even moderately overweight, your symptoms will be accentuated. Losing excess weight can greatly improve the pain you feel in your foot. Your physiotherapist at Body Works Fitness & Physiotherapy can discuss weight loss strategies with you and if need be, refer you to a Nutritionist who can also assist with this goal. Often it is difficult to exercise and increase your energy expenditure to lose weight when you have a painful foot, however, there are several safe activity options that your therapist can discuss with you, such as stationary cycling or swimming.
Activity modification is an important part of our treatment at Body Works Fitness & Physiotherapy. Your physiotherapist will strongly advise you to avoid any activities that cause you discomfort while you still have symptoms. This may also mean resting for a short period from any sport you do, or at least decreasing your amount of activity over a period of time. Your physiotherapist will specifically guide you regarding the needed rest for your individual injury. This rest may seem quite difficult to achieve, however it is well known that without a relative rest for a painful foot, there is little chance for it to heal. A period of rest where the foot is not being aggravated also greatly improves the ability of any medication you may be taking, along with the physiotherapy treatment you are receiving, to assist the healing of the injury. Your physiotherapist will advise you when it is safe to slowly start back at your activity after your period of rest.
Pain relief and improved function are the two main changes patients report with effective treatment. It's not clear yet if these measures prevent or stop the foot deformity from occurring or getting worse. Some short-term studies (one year) show good results with mild to moderate AAFD (stages I and II deformity) using orthotic support, foot orthotics, and physiotherapy.
Unfortunately, not all AAFD will respond to the physiotherapy treatment we provide at Body Works Fitness & Physiotherapy especially if your foot is in stage 3 or 4 of deformity. Any sign of increasing deformity may be an indication that surgery is needed. Careful monitoring over time is needed to assure the best timing for surgery. Waiting too long can mean a less successful surgical result. Your physician or physiotherapist will refer you on to an Orthopaedic Surgeon to discuss a more aggressive treatment as soon as they feel that conservative treatment is not improving your symptoms of AAFD or if they note an increase in deformity is occurring.
Body Works Fitness & Physiotherapy provides services for physiotherapy in Baie Verte and Springdale.
Surgery
When conservative care fails to control symptoms and/or deformity, then surgery may be needed. The goal of surgical treatment is to obtain good alignment while keeping the foot and ankle as flexible as possible.
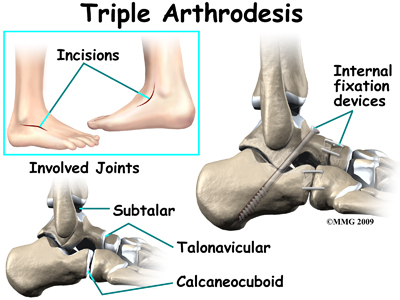
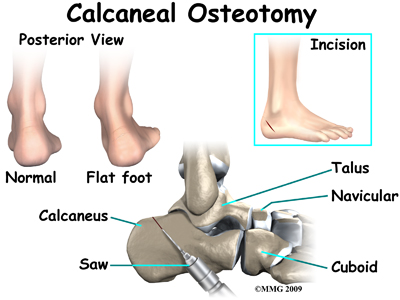
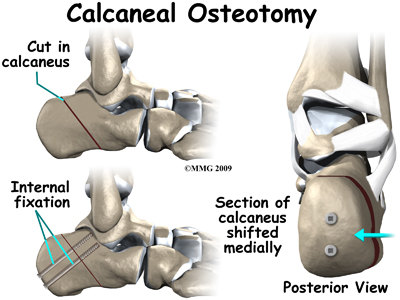
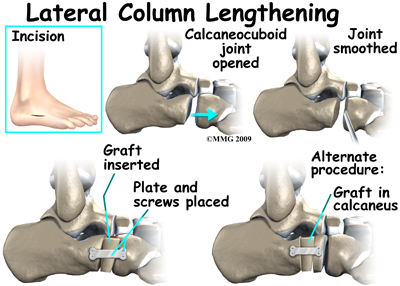
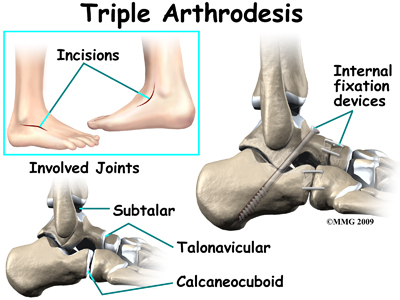
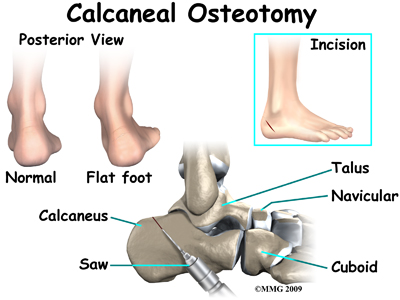
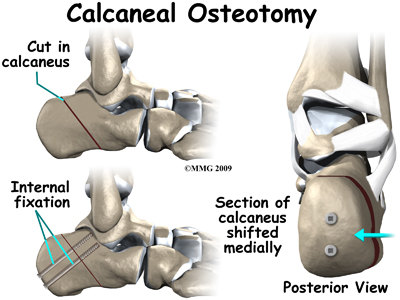
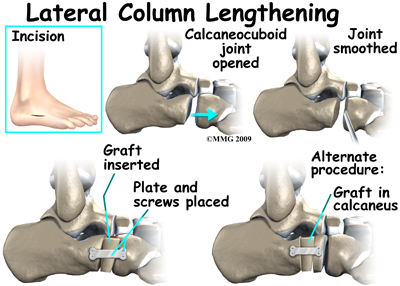
The most common surgical procedures used with this condition include arthrodesis (fusion), osteotomy (cutting out a wedge-shaped piece of bone), and lateral column lengthening. Lateral column lengthening involves the use of a bone graft at the calcaneocuboid joint, which helps restore the medial longitudinal arch (arch along the inside of the foot).
AAFD resulting from a torn tendon or spring ligament will be repaired or reconstructed. Other surgical options include tendon shortening or lengthening, or the surgeon may move one or more tendons. This procedure is called a tendon transfer. A tendon transfer uses another tendon to help the posterior tibial tendon function more effectively and to support the bones of the foot.
It's not clear yet from research evidence which surgical procedure works best for this condition. A combination of surgical treatments may be needed. It may depend on your age, type and severity of deformity and symptoms, and your desired level of daily activity. Studies do show, however, that long-term results of just reconstructing the posterior tibial tendon have been disappointing. As much as a 50 per cent failure rate has been reported which is likely because of the complexity of soft tissue interactions needed to maintain structural integrity of the foot. Reconstructing the spring ligament complex or using an osteotomy to lengthen the lateral side of the foot along with a tendon transplant is more likely to restore more normal foot and ankle movement with better results.
Post Surgical Rehabilitation
What should I expect as I recover?
Postoperative care will depend on the type of surgery you have. After a tendon transfer and/or osteotomy, you will be in a cast or removable brace for six weeks. In most cases, you won't be allowed to put weight on the foot during this time. This is especially true if you've had a tendon transfer or bone fusion. Physiotherapy at Body Works Fitness & Physiotherapy will begin after this time, or as soon as your surgeon indicates it is safe to begin. At this time you will probably be wearing a removable boot that you will take off to do your exercises. Eventually the removable boot will be replaced with a foot orthotic and regular lace-up shoes. As your foot heals from the surgery it is advised to avoid going barefoot when possible until the tissues have sufficiently healed, and the muscles have gained strength and motor control to assist in the position of the foot.
Post-surgical rehabilitation at Body Works Fitness & Physiotherapy will initially focus on minimizing the pain and swelling from the surgery. Similar to non-surgical rehabilitation, your physiotherapist may use modalities such as ice, ultrasound, or interferential current to accomplish this. They may also use gentle massage around the muscles of your foot and lower leg. Your physiotherapist will guide you on when to increase the weight-bearing load on your surgical foot. You will likely move from using two crutches down to just one, or a cane or stick, before going without any aid at all and putting full weight through your surgical foot.
One of the first exercises your physiotherapist will prescribe will be some gentle range of motion exercises for your foot and ankle to gradually regain full movement and to help decrease the swelling. These exercises may be as simple as ankle circles and pointing then pulling your toes and foot upward. The exercises should be done within a relatively pain-free motion, however, movement will be encouraged even if it causes a slight bit of discomfort as the movement itself can greatly assist with dispersing any swelling as well as improving the overall level of pain. Elevating your foot as often as possible in these early stages can also assist greatly with removing any swelling from the ankle. It is best to elevate your foot higher than your heart to allow gravity to assist with the fluid drainage.
A stationary bicycle can be very useful in the initial stages post-surgically to assist with gaining ankle range of motion and decreasing swelling, so, if you can, you will be encouraged to use one. Even if you are unable to fully rotate the pedals, the back and forth motion on the bike is an excellent method of slowly encouraging the ankle to regain its full range of motion.
As soon as you begin treatment at Body Works Fitness & Physiotherapy your physiotherapist will immediately prescribe exercises that address the proprioception of your foot, ankle and leg, as well as the alignment of the entire lower limb. Regaining a feel for the new position of your foot and arch is crucial to avoiding a recurrence of your symptoms. Simple strengthening exercises for the bottom of your foot, posterior tibialis muscle, as well as your hip muscles will also begin early on. Again, all exercises should be done within a relatively pain-free range of motion, however, some mild discomfort at the end ranges of motion may be felt as you begin to strengthen the muscles within their new range of motion.
It is crucial that you pay particular attention to the alignment of your arch, foot, ankle, and lower limb as you perform any of the exercises your physiotherapist prescribes. Poor alignment of any of these areas can begin re-creating a situation where you are again prone to AAFD symptoms. Your physiotherapist will repetitively remind you to be conscious of the overall alignment of the entire lower limb during both the rehabilitation exercises you do at Body Works Fitness & Physiotherapy as well during everyday activities such as walking and stair climbing.
Significant improvement in your foot after surgery occurs gradually over a four-to-six month period of time. During that time, your physiotherapist will progress your exercise program, but your appointments at Body Works Fitness & Physiotherapy will decrease in frequency. For those patients who have had a fusion, there will be some stiffness and loss of motion in the foot and/or ankle, so this should be expected. The amount and location of the stiffness depends on which bones were fused together.
Some prolonged swelling and discomfort are not uncommon even six to 10 months after the surgery. Standing on your feet for a long time or walking long distances can also cause foot pain or discomfort. Eventually these symptoms will disperse.
Returning to regular activities will occur slowly over a period of approximately 6-8 months. Your physiotherapist will guide you regarding the appropriate time to add more aggressive activities to your exercise and rehabilitation regime. If you are eager early on to get back to some cardiovascular activity, your physiotherapist can advise you regarding a safe intensity and duration of non-weight bearing cardiovascular activities such as swimming or cycling, and will also advise you on when it is safe to return to more aggressive activities for your foot and ankle such as jogging.
Generally post-surgical rehabilitation for AAFD at Body Works Fitness & Physiotherapy goes extremely well, however, if your pain lasts longer than it should or your rehabilitation is not progressing as quickly as your physiotherapist feels it should be, they will ask you to follow up with your surgeon to ensure there are no complicating factors impeding your recovery.
Body Works Fitness & Physiotherapy provides services for physiotherapy in Baie Verte and Springdale.
Portions of this document copyright MMG, LLC.









 At first you may notice pain and swelling along the medial (big toe) side of the foot. This is where the posterior tibialis tendon travels from the back of the leg under the medial ankle bone to the foot. As the condition gets worse, tendon failure may occur, and ligament laxity will worsen, causing the pain to get worse. Some patients also experience pain along the lateral (outside) edge of the foot and ankle, particularly as a deformity develops.
At first you may notice pain and swelling along the medial (big toe) side of the foot. This is where the posterior tibialis tendon travels from the back of the leg under the medial ankle bone to the foot. As the condition gets worse, tendon failure may occur, and ligament laxity will worsen, causing the pain to get worse. Some patients also experience pain along the lateral (outside) edge of the foot and ankle, particularly as a deformity develops.